
In 2011, President Obama signed the Food Safety Modernization Act, and the Food and Drug Administration (FDA) has proposed new regulations. FDA understands that limited information about pathogens in food is the root of the food safety problem:
“In an idealized perfectly competitive market in which consumers and producers both have sufficient information, the optimal level of production of foods that are manufactured, processed, packed or held by food facilities will be provided at an optimal level of safety. In real markets, however, consumers and producers may not have sufficient information on the safety attributes of foods….Currently, the legal system does not ensure the optimum level of safety for foods because consumers who become ill often do not know the reason for, or source of, their illness. Even in cases where consumers are aware that their illness was contracted from a specific food, it is often difficult to determine who is ultimately responsible for their illness, since the particular source of contamination is not known in many circumstances…. In sum, the imperfect information about the risk associated with food covered by the regulation means that neither the legal system nor the marketplace may be able to provide adequate economic incentives for the production of safe food. The Government may therefore be able to improve social welfare through targeted regulation.” (FDA, 2013, pp. 2-3).
The cornerstone of the food safety problem is that consumers cannot detect pathogens by either sight or smell. Lack of information is a serious problem for preventing and treating acute foodborne illness caused by pathogens, but it is even more challenging to link the Long Term Health Outcomes (LTHOs) associated with acute foodborne illness to the causative food source.
In 2011, the Centers for Disease Control and Prevention (CDC) updated its estimates of foodborne illness by reviewing medical databases that included foodborne illness symptoms (Scallan et al., 2011a, b). The CDC estimates that foods consumed in the United States cause 47.8 million acute illnesses annually. The CDC acknowledges that these acute foodborne illnesses can cause Long Term Health Outcomes, but does not identify or quantify LTHOs.
| Cause | Illnesses | Hospitalizations | Deaths |
| Major known pathogens1 | 9.4 million/ 20% | 56 thousand/ 44% | 1,351/ 44% |
| Unspecified agents2 | 38.4 million/ 80% | 72 thousand/ 56% | 1,686/ 56% |
| Total acute illness | 47.8 million/ 100% | 128 thousand/ 100% | 3, 037/ 100% |
| Long Term Health Outcomes | Acknowledged, but no identification of specific LTHOs | ||
In 2013, CDC published a landmark study analyzing foodborne illness outbreaks from 1998 to 2008 with an implicated food vehicle and a pathogen (Painter et al., 2013). In this 11-year period, the CDC confirmed only 271,974 outbreak illnesses where the food vehicle was identified with a single pathogen. These outbreaks encompass both those with a “confirmed” food source as well as outbreaks with a “suspect” food source. However, foodborne illnesses discovered in outbreaks are only a small percentage of all the total cases of acute foodborne illness. Painter et al. (2013) state: “…attributing all illnesses to specific foods is challenging because most agents are transmitted through a variety of foods, and linking an illness to a particular food is rarely possible except during an outbreak.”
On an annual basis, there are 24,745 of these outbreak illnesses per year linked to a food. However, outbreak illnesses are linked to a suspect/confirmed food in only 0.05% of the estimated 47.8 million U.S. annual foodborne illnesses, meaning that 99.95% of acute illnesses cannot be linked to the causative food.
Physicians and epidemiologists know that foodborne pathogens can cause acute illness, and by the 1980s, physicians became aware that acute foodborne illness can extend to a variety of LTHOs. These human LTHOs are a varied group and have no known cause, or a range of causes. Two common pathogens, Salmonella and E. coli O157:H7, illustrate two routes for discovering LTHOs of foodborne pathogens. Note that these discoveries occurred while epidemiologists were investigating acute foodborne illness outbreaks and their outcomes.
Scientific research has established that most foodborne pathogens have LTHOs that can have a wide range of health outcomes, some with life-long consequences (Roberts, Kowalcyk, and Buck, 2011). The range of LTHOs is very diverse: infections of the heart, brain, lung, gall bladder, spleen, intestines, muscles, pancreas, nervous system, and blood. Based on self-reported survey results from residents of Minnesota and Oregon who suffered a foodborne illness, links to reactive arthritis symptoms were established. The results, by pathogen, are: Salmonella (15%), Yersinia (14.3%), Campylobacter (12.7%), Shigella (9.7%), and E. coli O157:H7 (8.9%) (Townes et al., 2008). In addition, another study provided data on reactive arthritis and the probabilities of life-long joint or back pain (Raybourne et al., 2000).
| Foodborne Pathogen | Medical Cases of Long-Term Health Outcomes (LTHOs) |
| Campylobacter | Paralysis (Guillian-Barré Syndrome), reactive arthritis, carditis, cholecystitis, endocarditis, meningitis, pancreatitis, septicemia |
| E. coli O157:H7 | Kidney failure (Hemolytic Uremic Syndrome), neurological problems, diabetes, gallstones, hypertension, irritable bowel syndrome, intestinal strictures, pneumonia |
| Listeria monocytogenes | Meningitis, neurological dysfunction, sepsis |
| Salmonella | Reactive arthritis, aorititis, cholecystitis, colitis, endocarditis, epididymo-orchitis, meningitis, ostemyelitis, pancreatitis, septicemia, splenic abscess |
| Shigella | Kidney failure (Hemolytic Uremic Syndrome), reactive arthritis, splenic abscess, synovitis |
| Yersinia | Cholangitis, liver and splenic abscesses, lymphadenitis, pneumonia, pyomyositis, reactive arthritis, septicemia, spondylitis |
| Toxoplasma gondii | Encephalitis, moderate to severe mental retardation, blindness, schizophrenia, self-directed violence |
| Extraintestinal E. coli | Urinary tract infections |
| Many bacterial pathogens | Antibiotic resistance acquired during on-farm production of food animals |
More recently, scientific information links three new types of illness to foodborne pathogens: mental illness, urinary tract infections, and infections due to antibiotic-resistant foodborne bacterial pathogens.
Adult cases of mental illness in several countries have been linked to the parasite, Toxoplasma gondii. The epidemiology gold standard for making these linkages is a prospective study where an exposed cohort is followed over time to document what illnesses they develop in comparison to a non-exposed cohort. Several studies in the United States and Europe have examined patient levels of T. gondii antibodies relative to their risk for various mental health conditions, such as schizophrenia (Pedersen et al., 2011 and 2012, and Flegr, 2013). The two primary sources of T. gondii for human illness in the United States are lightly cooked meats—primarily pork, lamb, and venison—and exposure to cat feces (CDC, 2013). Half of the human cases of toxoplasmosis are estimated to be foodborne (Scallan et al., 2011b).
In 2012, Racicot Bergeron et al. published a path-breaking study linking chicken to human urinary tract infections (UTIs). Extraintestinal pathogenic E. coli (ExPEC) causes the majority of UTIs in the United States. Given the statistically significant genetic similarities between human and chicken E. coli isolates, the researchers concluded that “….ExPEC transmission from food animal sources is likely to be implicated in human infections and that chicken is a major reservoir” (Racicot Bergeron et al., 2012).
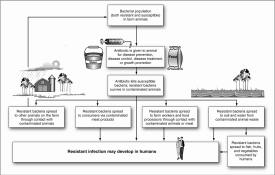
A 2011 Government Accountability Office (GAO) report found several pathways whereby antibiotic-resistant bacteria spread from animals to cause diseases in humans. The annual report of the National Antibiotic Resistance Monitoring System revealed “…more than half of samples of ground turkey, pork chops and ground beef collected from supermarkets for testing by the federal government contained a bacteria resistant to antibiotics…” (Strom, 2013).
For all three of these recent LTHOs, it is not yet possible to estimate what percent are caused by food. However, the study on UTIs illustrates that pathogen testing data can indicate what pathogens are in foods in production and in the marketplace. This information could be used to alert consumers, industry, and regulators to take actions to reduce contamination or take precautions to avoid the product.
In 1997, Buzby and Roberts compared the costs of acute foodborne illness vs. LTHOs for several foodborne pathogens. For some pathogens, the LTHOs are more costly than the total for acute illness and death. In 2012, Hoffman, Batz, and Morris estimated that 14 foodborne pathogens caused $14.1 billion in the cost of illness, and loss of over 61,000 Quality Adjusted Life Years (QALYs) annually. Also in 2012, Scharff estimated the annual cost of U.S. foodborne illness from $51 billion to $78 billion using two estimation methods based on cost of illness and monetized QALYs. Both 2012 studies included a few LTHOs in their estimates.
In 2013, FDA’s Preliminary Regulatory Impact Analysis for the Food Safety Modernization Act proposed regulations for processed foods evaluated only three LTHOs for foodborne pathogens: paralysis for Campylobacter, kidney failure for E. coli O157:H7, and reactive arthritis for three pathogens (FDA, 2013). Reactive arthritis is estimated to cause illness for only one year, however, which excludes the longer term outcomes experienced by some Canadian Mounties five years after acute salmonellosis (Thomson et al., 1995).
For the three recently discovered LTHOs discussed above, the percentage attributed to food is unknown today. But each imposes substantial costs on society:
In conclusion, while LTHOs are relatively rare, their potentially life-long impacts can be more costly than acute illnesses and deaths for a particular pathogen (Buzby and Roberts, 1997). Economists need to take LTHOs seriously, especially since scientific discoveries keep expanding the list of foodborne LTHOs.
The public good aspect of food safety is heightened by the lack of information about acute foodborne illnesses caused by pathogens and the associated LTHOs. But is this a problem that the United States public wants addressed? What options are available to deal with this issue? Three pieces of evidence indicate that the public wants more food safety:
Government, industry, and consumers cannot make well-informed decisions about food supply risks if only 0.05% of foodborne illnesses are linked to the food and the pathogen. There are actions that could improve information in the marketplace, and these would improve efficiency if the costs of the information are offset by the reduction in foodborne illness. There are several options for improving information on pathogens in the U.S. food supply chain:
Option 1: Expanded financial support of databases and research by CDC, USDA, and FDA in the National Antibiotic Resistance Monitoring System, and the new Interagency Food Safety Analytics Collaboration (IFSAC). IFSAC’s initial objective has been to attribute the food source for four important pathogens, Campylobacter, Salmonella, E. coli O157, and Listeria (IFSAC, 2012). Perhaps, other Federal data collected on pathogens in foods can be added to this national database and the latest pathogen testing methods used (Eppinger et al., 2011).
Option 2: Another option is to create a new farm-to-table database to trace types of pathogens to specific farms, food companies, and products, hopefully with the cooperation of industry and inclusion of company data. Such a database with “blinded” company data is valuable input for industry in its standard-setting activities for pathogens in supplier contracts and in monitoring a company’s own performance. A paper in the prestigious journal, Proceedings of the National Academies of Science, analyzes how new pathogen testing technologies can better identify the pathogen strains in the food sources causing an outbreak (Eppinger et al., 2011).
Option 3: A more limited option that relies on improving the legal liability system is legislation to create a national product liability database to document the outcomes of all product liability court cases, including out-of-court settlements for foodborne illness cases (Buzby, Frenzen, and Rasco, 2001). Repeat violators could then be identified to some extent and class action suits be based on out-of-court settlements for cases initially brought to the court. This action would increase economic incentives for greater industry control of foodborne pathogens.
Option 4: Creation of a Cabinet-level Consumer Protection Agency was proposed as early as the Johnson Administration when Esther Peterson was the White House Consumer Advocate (NBCNews, 2013). If a Cabinet-level position, or perhaps an independent agency, were created, this Consumer Protection Agency could promote and oversee collection of pathogen data in the U.S. food supply.
Two overarching questions remain. Which of these four options is most likely to be most cost-beneficial to the U.S. economy? Option 1 may be the easiest to implement, since the structure already exists in IFSAC. However, are there other, more pressing uses of the taxpayers’ money that are more cost-beneficial? The lack of information linking pathogens to the U.S. food supply cannot be denied as only 0.05% of current human acute illnesses can be linked to pathogens today. LTHOs, which can be as economically important as acute illnesses, have an even more tenuous link to the food that causes the illness. Information is a critically important method of improving food safety incentives and promoting efficiency in controlling pathogens in the U.S. food supply.
Buzby, J.C., Frenzen, P., and Rasco, B. (2001). Product Liability and Microbial Foodborne Illness, Agricultural Economic Report No. (AER-799), ERS, USDA, 41 pages. Available online at http://ers.usda.gov/publications/aer-agricultural-economic-report/aer799.aspx.
Buzby, J.C., and Roberts, T. (1997). Guillain-Barré Syndrome increases foodborne disease costs, FoodReview, Washington, DC: US Department of Agriculture, Economic Research Service, 20 (3), pp. 36-42. Available online at http://webarchives.cdlib.org/sw16m34098/http://www.ers.usda.gov/publications/foodreview/sep1997/sept97h.pdf.
Centers for Disease Control and Prevention (CDC) website on toxoplasmosis. Available online at http://www.cdc.gov/parasites/toxoplasmosis/epi.html.
Ellison, B.E. and Lusk, J.L. (2nd quarter 2011). Taxpayer preferences for USDA expenditures, Choices. Available online at http://www.choicesmagazine.org/choices-magazine/submitted-articles/taxpayer-preferences-for-usda-expenditures.
Eppinger, M., Mammel, M.K., Leclerc, J.E., Ravel, J., and Cebula, T.A. (2011). Genomic anatomy of Escherichia coli O157:H7 outbreaks, Proceedings of the National Academies of Science, 108, (50), 20142-20147; published ahead of print November 30, 2011, Available online at http://dx.doi.org/10.1073/pnas.1107176108
Flegr, J. (2013). Review: influence of latent Toxoplasma infection on human personality, physiology and morphology: pros and cons of Toxoplasma-human model in studying the manipulation hypothesis. The Journal of Experimental Biology, 216(1), 127-133.
Food and Drug Administration (2013). Preliminary Regulatory Impact Analysis for the processed food rule. Available online at http://www.fda.gov/downloads/Food/GuidanceRegulation/FSMA/UCM334117.pdf
Government Accountability Office (2011). Antibiotic Resistance: Agencies Have Made Limited Progress Addressing Antibiotic Use in Animals, GAO-11-801, 1-77. Available online at http://www.gao.gov/products/GAO-11-801.
Hoffmann S., Batz M.B., and Morris Jr. J.G. (July 2012). Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens. Journal of Food Protection, 75(7):1292-302. Available online at http://dx.doi.org/10.4315/0362-028X.JFP-11-417.
Interagency Food Safety Analytics Collaboration (January 2012). Strategic plan for foodborne source attribution. Available online at http://www.resolv.org/site-foodsafety/files/2011/12/IFSAC_Draft_Strategic_Plan_Attribution1.pdf
Kurtz, M.M. (2013). A social salve for schizophrenia, Scientific American Mind, 24(1), 62-67.
NBCNews (April 26, 2013). Obama should restore consumer czar office. Available online at http://redtape.nbcnews.com/_news/2009/01/16/6345803-obama-should-restore-consumer-czar-office?lite
Painter J.A., Hoekstra R.M., Ayers T., Tauxe R.V., Braden C.R., and Angulo F.J. (2013). Attribution of foodborne illnesses, hospitalizations, and deaths to food commodities by using outbreak data, United States, 1998–2008. Emerging Infectious Diseases [Internet]. 19(3), ahead of print [accessed on February 5, 2013]. Available online at http://dx.doi.org/10.3201/eid1903.111866
Pedersen, M.G., Mortensen, P.B., Norgaard-Pedersen, B., and Postolache, T.T. (2012). Toxoplasma gondii infection and self-directed violence in mothers. Archives of General Psychiatry, 69(11), 1123-30.
Pedersen, M.G., Stevens, H., Pedersen, C.B., Norgaard-Pedersen, B., Mortensen, P.B. (2011). Toxoplasma infection and later development of schizophrenia in mothers. American Journal of Psychiatry, 168(8), 814-821.
Racicot Bergeron C., Prussing C., Boerlin P., Daignault D., Dutil L., Reid-Smith R.J. (2012). Chicken as reservoir for extraintestinal pathogenic Escherichia coli in humans, Canada. Emerging Infectious Diseases 18(3), 415-421. Available online at http://dx.doi.org/10.3201/eid1803.111099.
Rangel, J.M., Sparling, P.H., Crowe, C., Griffin, P.M., and Swerdlow, D.L. (2004). Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982–2002. Emerging Infectious Diseases. Available online at http://wwwnc.cdc.gov/eid/article/11/4/04-0739.htm DOI:10.3201/eid1104.040739
Raybourne, R.B., Williams, K.M., Roberts, T. and the ArthritisWorking Group (2000). Food poisoning: economic considerations, In L. Trugo and P. Finglas (eds.), Encylopedia of Food Sciences and Nutrition, Elsevier Science, Ltd., pp. 2672-82.
Roberts, T., Kowalcyk, B., and Buck, P. (2011). The Long-Term Health Outcomes of Selected Foodborne Pathogens. Grove, City, Pennsylvania: Center for Foodborne Illness Research and Prevention. Available online at http://www.foodborneillness.org/images/stories/cfi_pdfs/CFI_LTHO_PSP_report_Nov2009_050812.pdf.
Scallan E., Griffin P.M., Angulo F.J., Tauxe R.V., and Hoekstra R.M. (2011a). Foodborne illness acquired in the United States—unspecified agents. Emerging Infectious Diseases, 17(1), 16-22. Available online at http://dx.doi.org/10.3201/eid1701.P21101.
Scallan E., Hoekstra R.M., Angulo F.J., Tauxe R.V., Widdowson M.A., and Roy S.L. (2011b). Foodborne illness acquired in the United States—major pathogens. Emerging Infectious Diseases, 17(1), 7–15. Available online at http://dx.doi.org/10.3201/eid1701.P11101.
Scharff, R.L. (2012). Economic burden from health losses due to foodborne illness in the United States. Journal of Food Protection, 75(1), 123-131. Available online at http://dx.doi.org/10.4315/0362-028X.JFP-11-058.
Strom, S. (2013). Report on U.S. meat sounds alarm on resistant bacteria. The New York Times April 16. Available online at http://nyti.ms/111Mxq6.
Thomson, G.T., DeRubeis, D.A., Hodge, M.A., Rajanayagam, C., and Inman, R.D. (1995). Post-Salmonella reactive arthritis: late clinical sequelae in a point source cohort. American Journal of Medicine, 98, 13–21.
Torgerson, P.R., and MacPherson, C.N.L., (2011). The socioeconomic burden of parasitic zoonoses: global trends. Veterinary Parasitology, 183, 79-95.
Townes, J.M., Deodhar, A.A., Laine, E.S., Smith, K., Krug, H.E., Barkhuizen, A., Thompson, M.E., Cieslak, P.R., and Sobel, J. (2008) Reactive arthritis following culture-confirmed infections with bacterial enteric pathogens in Minnesota and Oregon: a population-based study. Annals of the Rheumatic Diseases 67:1689-1696.
Unnevehr, L.J. (2006) Food Safety as a Global Public Good: Is There Underinvestment? Plenary Paper, International Association of Agricultural Economists Conference, Australia, August 12-18. Available online at http://ageconsearch.umn.edu/handle/25733.
U.S. Department of Agriculture, FY 2010 Budget Summary and Annual Performance Plan. Available online at http://www.obpa.usda.gov/budsum/FY12budsum.pdf.