
The current U.S. Department of Agriculture (USDA) strategic plan, which guides many of its grant programs, highlights the connection between financial sustainability of food producers, supply of fresh local food to consumers, and improved nutritional and health outcomes (U.S. Department of Agriculture, 2014). Achieving these goals requires an integrated and transdisciplinary approach to tackle the interactions between components of the complex food system and human health (Nesheim, Oria, and Yih, 2015). There is limited empirical evidence to date about the relationship between producers’ financial sustainability and public health outcomes. In particular, there is little understanding of whether financial security and diet-related health outcomes can interact positively (Sitaker et al., 2014).
To fill these knowledge gaps, our team of researchers—spanning the fields of nutrition, public health, and economics—developed an innovative project that integrates increased access to fresh produce for low-income households with entrepreneurial food systems innovation. This project, called Community Supported Agriculture Cost-offset Intervention to Prevent Childhood Obesity and Strengthen Local Agricultural Economies, is funded by the USDA Agriculture and Food Research Initiative (AFRI) project. Its intent is to integrate research, extension, and education to examine subsidized or “cost-offset” community supported agriculture (CO-CSA) participation as a strategy for improving dietary quality among low-income families, help at-risk children achieve and maintain healthy body weights, and support vibrant agricultural economies.
This is the first transdisciplinary initiative to rigorously evaluate dietary outcomes resulting from the direct-to-consumer (CSA) sales of fresh produce to low-income families, combined with nutrition education, over multiple years as well as assessing impacts on the local economy. It draws on research related to obesity, fruit and vegetable consumption, food access in rural areas (particularly access to fresh produce), and farm viability in direct-to-consumer market channels. This article focuses on the formative research component of the larger study. Data were collected from CSA participants, extension educators, and farmers. Findings of the formative evaluation align with both anecdotal and academic findings: involvement, freshness, value, and variety are important to increasing familiarity and use of fruits and vegetables.
More than a third of American children and adolescents are obese or overweight, creating alarming social, medical, and economic costs to society as a growing number of children experience costly and debilitating obesity-related health issues like type 2 diabetes and cardiovascular disease (Ogden et al., 2014). These problems may be compounded by other costly health conditions throughout life, including high blood pressure, osteoarthritis, certain cancers, stroke, and heart disease (National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012). Rates of obesity and chronic disease are higher among low-income and rural populations, the latter of which are more likely to live in poverty compared to urban populations (Lobmayer and Wilkinson, 2002; Gamm et al., 2003; U.S. Department of Agriculture, Economic Research Service, 2014). Yet Americans currently eat less than two-thirds of the recommended amounts of fruit and vegetables, as well as lower than recommended levels of nutrient-dense dark green and orange vegetables (U.S. Department of Agriculture and U.S. Department of Health and Human Services, 2010).
Individuals with low socioeconomic status, food insecurity, and rural residence have even lower levels of fruit and vegetable consumption, partly due to less access to fresh, affordable foods (U.S. Department of Agriculture and U.S. Department of Health and Human Services, 2010; Guenther et al., 2006; Bowman, 2007; Lallukka et al., 2010; Hanson and Conner, 2014; Lutfiyya, Chang, and Lipsky, 2012; Liu et al., 2012; Larson, Story, and Nelson, 2009).
Moderate evidence suggests that increasing fruit and vegetable consumption in adults can lead to weight loss when combined with reduced consumption of energy-dense foods, which may be effective in maintaining a healthy weight (Boeing et al., 2012; Mytton et al., 2014). Evidence of an association between fruit and vegetable consumption and weight development in children and adolescents is much weaker, but some observational and epidemiological studies have shown that consuming more fruits and vegetables is associated with lower body weight in children (Boeing et al., 2012; Tohill et al., 2004; Lin and Morrison, 2002). When substituted for energy-dense foods or combined with other strategies—such as increasing physical activity—increased fruit and vegetable consumption may prevent weight gain or promote weight maintenance (Ledoux, Hingle., and Baranowski, 2011; Rolls, Ello-Martin, and Tohill, 2004).
These relationships are important considerations for long-term child obesity prevention because we know that behaviors established in childhood and adolescence often persist into adulthood and that parental eating behavior is a potent influence on children’s diets (Kelder et al., 1994; Mikkilä et al., 2004; Poti, Duffey, and Popkin, 2014). Collectively, this evidence supports integrated, family-based strategies for childhood obesity prevention that include increasing access to and consumption of fruits and vegetables, which can displace energy-dense foods and beverages.
Like other direct-to-consumer outlets, CSAs have the potential to improve physical and financial access to fresh produce (Cooley and Lass, 1998). CSAs allow consumers pay upfront for a “share” of a farmer’s crop, receiving fresh produce regularly as it is harvested during the growing season. CSA produce can cost significantly less than similar types and amounts of produce bought at the grocery store (Perez, Allen, and Brown, 2003; Russell and Zepeda, 2008; Brehm and Eisenhauer, 2008). However, findings on the profitability of CSAs to the farmer are contradictory: In some cases CSAs are more profitable than wholesale accounts but, in others, farmers reported dissatisfaction with economic returns (Stagl, 2002; Jablonski, Perez-Burgos, and Gomez, 2011).
CSA membership has been associated with increased willingness to try new produce and greater consumption of meals at home (Russell and Zepeda, 2008; Andreatta, Rhyne, and Dery, 2008). It may also result in increases in the quantity and variety of fruits and vegetables consumed by CSA members (Russell and Zepeda, 2008; Uribe, Winham, and Wharton, 2012; Allen et al., 2016). Though logistical barriers to CSA share pick up and unfamiliarity with some CSA vegetables are reported by low-income families as rationale for lower participation, CSAs may be feasible and acceptable to low-income participants under the right conditions.
Subsidized CSA shares, convenient pick-up locations, and complementary nutrition education are strategies that researchers and educators have employed to increase participation among low-income families with children (Hayden and Buck, 2012; Healthy Food for All, 2014; Northeast Organic Farming Association of Vermont, 2014; Harnack et al., 2016; Quandt et al., 2013; Hoffman et al., 2012). Farmers can use a variety of strategies to help potential limited-resource members overcome income barriers, including accepting Supplemental Nutrition Assistance Program benefits (SNAP), payment plans, working shares, subsidies from grants or full-pay members, low-cost shares, transportation assistance, and bartering (Forbes and Harmon, 2008). Farmers have been shown to benefit from CSAs via improved financial security, decreased time and money spent on marketing (particularly during their growing season), and reduced production costs (Saulny, 2008; Stagl, 2002; LeRoux et al., 2010; Sabih and Baker, 2000; Cohen and Derryck, 2011; Jablonski, Perez-Burgos, and Gomez, 2011; Hardesty, 2010). By accommodating low-income participants through share subsidies, farmers can potentially expand their market reach.
Recent studies have shown positive changes in attitudes and consumer behavior toward fruit and vegetables among low-income CSA members (Harnack et al., 2016; Quandt et al., 2013; Hoffman et al., 2012) and among CSA members in general (Curtis, Allen and Ward, 2015). Nonetheless, aside from the rigorous dietary outcome measures reported in Harnack et al. (2016), who studied subsidized incentives for fruit and vegetable purchases, there is limited empirical evidence for the benefits of longer-term CSA membership on dietary quality, particularly among low-income families (McCormack et al., 2010; Hedden, 2011). Similarly, the economic impact of CO-CSAs on farm profitability has not been adequately studied.
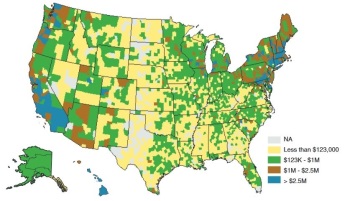
Source: Low et al., 2015
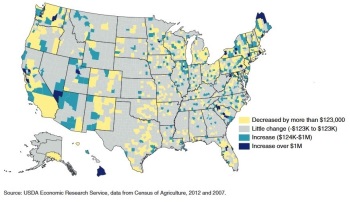
Source: Low et al., 2015
The formative research presented here includes participation in CSAs with different business models in New York, North Carolina, Vermont, and Washington. The quantity and value of direct-to-consumer sales varies considerably across the states and communities participating in this research and captures most of the range of variation in sales seen across the United States. Direct-to-consumer sales are consistently high across all Vermont counties; New York and Washington both have some counties with lower and some with higher direct-to-consumer sales; overall, North Carolina counties have lower direct-to-consumer sales (Low et al., 2015).
Between 2007 and 2012, all four states have seen areas of growth, stability, and decline in direct-to-consumer sales. By including multiple states and three U.S. regions, we aim to increase the likelihood that our research results will be relevant and transferable nationally to other communities trying to increase farmer viability and decrease childhood obesity by increasing fruit and vegetable consumption through direct-to-consumer markets.
We used formative research methods to develop an increased understanding of CSA beliefs, perceptions, and practices among key intervention stakeholder groups. This method leads to proper targeting and appropriate strategies for the intervention, which began during the 2016 growing season. We performed qualitative interviews in each of the four intervention states with twenty-four CSA farmers, forty-one parents in low-income households, and twenty community health educators. We chose respondents using sampling matrices to ensure that they represented a diversity of characteristics (such as farm experience with cost offset mechanisms and children of appropriate age in low-income households) that were of relevance to the intervention.
These interviews described the perceived benefits, opportunities, consequences, and barriers to the CO-CSA model and the proposed intervention. We used these findings to design the intervention, guided by emergent themes related to (i) general beliefs and attitudes about produce and farming, (ii) perceptions of CSAs, and (iii) perceptions of successful nutrition education curricula.
A transdisciplinary team with a breadth of perspectives requires deep discussion and consideration of the benefits and drawbacks of quasi-experimental comparison as opposed to randomized control designs, the appropriate level of randomization (individual versus community), and a host of measurement issues. Some of these challenges are outlined in the literature (Hamermesh, 2001; Kolodinsky et al., 2009; Kolodinsky and Goldstein 2011; Sturm, 2005; McKinnon et al., 2009). This consideration has allowed us to create a rigorous research design that integrates these perspectives and meets the demands of many fields.
A randomized experimental design with a delayed-intervention control group will maximize our ability to rigorously measure program impacts on low-income households while meeting high ethical standards for responsible community nutrition research (allowing all participants to ultimately benefit from the program). Individual 1:1 randomization is implemented within community clusters to produce equivalent intervention and control groups while also acknowledging that agriculture requires planning well in advance of the CSA season and that our CSA partner farms need to know how many shares are required in each year of the longitudinal intervention study.
Our data collection approach attempts to capture a broad range of information; therefore, we have employed a diverse array of data collection methods, including qualitative interviews and focus groups; longitudinal quantitative on-line surveys; in-person physical measurements of children and adults; on-line completion of 24-hour dietary recalls for children; on-line and paper process evaluation surveys from educators and participants; skin carotenoid measures using new, non-invasive technology; and end-of season interviews with farmers, educators, and participant parents. These multiple data sources provide a range of perspectives.
The rationale for integrating different disciplines in food system research has been clearly articulated, but there is limited evidence on food systems programs and policies that align with nutrition goals. Looking to the future, this project seeks to generate new evidence on what programs best serve the needs of both low-income families and local agricultural economies. In addition to studying impacts, the practical, real-world nature of this project will facilitate the development of a nuanced understanding of the incentives and disincentives for farmers and consumers in a CO-CSA model. Our team designed evaluation instruments collaboratively and iteratively to shed light on a range of implementation factors, including the perspectives of key stakeholders on how the intervention is working. Information gathered will help identify areas where targeted action could enhance nutrition and health as well as economic outcomes. We plan to share our program experiences so that others may benefit from what we learn.
Many opportunities exist for researchers in agriculture, nutrition, health, and community development to interact in projects such as this, which require deep inquiry, reflection, and problem-solving. All study materials—from data collection instruments to participant reminder messages and our logo—have been developed and refined collectively, and issues that have arisen have been resolved through discussion and critical reflection among research team members and institutions. The extended project time frame (five years) allows us to grow together while working on a tangible project that demands diverse expertise and perspectives.
Allen IV, J. E., J. Rossi, T. A. Woods, T. A., and A. F. Davis. 2016. “Do Community Supported Agriculture Programmes Encourage Change to Food Lifestyle Behaviours and Health Outcomes? New Evidence from Shareholders.” International Journal of Agricultural Sustainability 15: 70–82.
Andreatta, S., M. Rhyne, and N. Dery. 2008. “Lessons Learned from Advocating CSAs for Low-Income and Food Insecure Households.” Southern Rural Sociology 23: 116–148.
Boeing, H., A. Bechthold, A. Bub, .S. Ellinger, D. Haller, A. Kroke, E. Leschik-Bonnet, M. J. Müller, H. Oberritter, M. Schulze, P. Stehle, and B. Watzi. 2012. “Critical Review: Vegetables and Fruit in the Prevention of Chronic Diseases.” European Journal of Nutrition 51: 637–663.
Bowman, S. 2007. “Low Economic Status Is Associated with suboptimal intakes of Nutritious Foods by Adults in the National Health and Nutrition Examination Survey 1999–2002.” Nutrition Research 27: 515–523.
Brehm, J. M., and B. W. Eisenhauer. 2008. “Motivations for Participating in Community- Supported Agriculture and Their Relationship with Community Attachment and Social Capital.” Southern Rural Sociology 23: 94–115.
Cohen, N., and D. Derryck. 2011. “Corbin Hill Road Farm Share: A Hybrid Food Value Chain in Practice.” Journal of Agriculture, Food Systems, and Community Development 1(4): 85–100.
Cooley, J. P., and D. A. Lass. 1998. “Consumer Benefits from Community Supported Agriculture Membership.” Review of Agricultural Economics 20: 227–237.
Curtis, K. R., K. Allen, and R. A. Ward. 2015. “Food Consumption, Attitude, and Behavioral Change among CSA Members: A Northern Utah Case Study.” Journal of Food Distribution Research 46(2): 3–16.
Forbes, C. B., and A. H. Harmon. 2008. “Buying into Community Supported Agriculture: Strategies for Overcoming Income Barriers.” Journal of Hunger and Environmental Nutrition 2(2–3): 65–79.
Gamm, L., L. Hutchison, B. Dabney, and A. Dorsey. 2003. Rural Healthy People 2010. Volume 2. College Station, TX: Texas A&M University, School of Public Health, Southwest Rural Health Research Center. Available online: https://sph.tamhsc.edu/srhrc/rhp2010.html
Guenther, P., K. Dodd, J. Reedy, and S. Krebs-Smith. 2006. “Most Americans Eat Much Less than Recommended Amounts of Fruits and Vegetables.” Journal of the American Dietetic Association 106: 1371–1379.
Hamermesh, D. “Time to Eat: Household Production under Increasing Income Inequality.” American Journal Agricultural Economics 89: 852–853.
Hanson, K. L., J. Kolodinsky, M. Gauger, A. Ammerman, S. B. Jilcott Pitts, M. Sitaker, and R. A. Seguin. 2016. “ Paper presented at American Public Health Association annual meeting, Denver, CO, 29 October–2 November.
Hanson, K. L., and L. M. Connor. 2014. “Food Insecurity and Dietary Quality in US Adults and Children: A Systematic Review.” American Journal of Clinical Nutrition 100: 684–692.
Hardesty, S. D. 2010. “Determining Marketing Costs and Returns in Alternative Marketing Channels.” Renewable Agriculture and Food Systems 25: 24–34.
Harnack, L., J. M. Oakes, B. Elbel, T. Beatty, S. Rydell, and S. French. 2016. “Effects of Subsidies and Prohibitions on Nutrition in a Food Benefit Program: A Randomized Clinical Trial.” JAMA Internal Medicine 176: 1610–1618.
Hayden, J., and D. Buck. 2012. “Doing community Supported Agriculture: Tactile Space, Affect and Effects of Membership.” Geoforum 43: 332–341.
Healthy Food for All. 2014. Building Community Health, Food Equity, and Farm Viability. Available online: http://www.healthyfoodforall.org/
Hedden, J. L. 2011. “The Effect of CSA Membership on Fruit and Vegetable Intake.” Master’s thesis, Colorado State University, Fort Collins.
Hoffman, J. A., T. Agrawal, C. Wirth, C. Watts, G. Adeduntan, L. Myles, and C. Castaneda-Sceppa. 2012. “Farm to Family: Increasing Access to Affordable Fruits and Vegetables among Urban Head Start Families.” Journal of Hunger and Environmental Nutrition, 7(2–3): 165–177.
Jablonski, B. R., J. Perez-Burgos, and M. Gomez. 2011. “Food Value Chain Development in Central New York: CNY Bounty.” Journal of Agriculture, Food Systems and Community Development, 1(4): 129–141.
Kelder, S. H., C. L. Perry, K. I. Klepp, and L. L. Lytle. 1994. “Longitudinal Tracking of Adolescent Smoking, Physical-Activity, and Food Choice Behaviors.” American Journal of Public Health 84: 1121–1126.
Kolodinsky, J., and R. A. Seguin. 2016. “ Paper presented at the AAEA annual meeting, Boston, MA, 31 July–2 August.
Kolodinsky, J., A. Goldstein, J. Hyman, and E. Roche. 2009. “Household Food and Beverage Purchasing.” Journal of the American Dietetic Association 9: 982–983.
Kolodinsky, J. M., and A. B. Goldstein. 2011, “Time Use and Food Pattern Influences on Obesity.” Obesity 19: 2327–2335.
Lallukka, T., Pitkäniemi, J., Rahkonen, O., Roos, E., Laaksonen, M., and Lahelma, E. 2010.” The Association of Income with Fresh Fruit and Vegetable Consumption at Different Levels of Education.” European Journal of Clinical Nutrition 64: 324–327.
Larson, N. I., M. T. Story, and M. C. Nelson. 2009. “Neighborhood Environments: Disparities in Access to Healthy Foods in the US.” American Journal of Preventive Medicine 36: 74–81.
Ledoux, T. A., M. D. Hingle, and T. Baranowski. 2011. “Relationship of Fruit and Vegetable Intake with Adiposity: A Systematic Review.” Obesity Reviews 12(501): e143-e150.
LeRoux, M. N., T. M. Schmit, M. Roth, and D. H. Streeter. 2010. “Evaluating Marketing Channel Options for Small-Scale Fruit and Vegetable Producers.” Renewable Agriculture and Food Systems 25: 16–23.
Lin, B.-H., and R. M. Morrison. 2002. “Higher Fruit Consumption Linked with Lower Body Mass Index.” Food Review. 25(3): 28–32.
Liu, J.-H., S. J. Jones, H. Sun, J. C. Probst, A. T. Merchant, and P. Cavicchia. 2012. “Diet, Physical Activity, and Sedentary Behaviors as Risk Factors for Childhood Obesity: An Urban and Rural Comparison.” Childhood Obesity 8: 440–448.
Lobmayer, P., and R. G. Wilkinson. 2002. “Inequality, Residential Segregation by income, and Mortality in US Cities.” Journal of Epidemiology and Community Health 56(3): 183–187.
Low, S. A., and S. Vogel. 2011. Direct and Intermediated Marketing of Local Foods in the United States. Washington, DC: U.S. Department of Agriculture, Economic Research Service, Economic Research Report 128, November.
Low, S. A., A. Adalja, E. Beaulieu, N. Key, S. Martinez, A. Melton, A. Perez, K. Ralston, H. Stewart, S. Suttles, S. Vogel, and B. B.R. Jablonski. 2015. Trends in U.S. Local and Regional Food Systems. Washington, DC: U.S. Department of Agriculture, Economic Research Service, Administrative Publication 68.
Lutfiyya, M. N., L. F. Chang, and M. S. Lipsky. 2012. “A Cross-Sectional Study of Us Rural Adults’ Consumption of Fruits and Vegetables: Do They Consume at Least Five Servings Daily?” BMC Public Health 12: 280.
McCormack, L. A., M. N. Laska, N. I. Larson, and M. Story. 2010. “Review of the Nutritional Implications of Farmers’ Markets and Community Gardens: A Call for Evaluation and Research Efforts.” Journal of the American Dietetic Association 110: 399–408.
McKinnon, R. A., J. Reedy, S. L. Handy, and A. B. Rodgers. 2009. “Measuring the Food and Physical Activity Environments: Shaping the Research Agenda.” American Journal of Preventive Medicine 36: S81–S85.
Mikkilä, V., L. Räsänen, O. Raitakari, P. Pietinen, and J. Viikari. 2004. “Longitudinal Changes in Diet from Childhood into Adulthood with Respect to Risk of Cardiovascular Diseases: The Cardiovascular Risk in Young Finns Study.” European Journal of Clinical Nutrition 58: 1038–1045.
Morgan, E. H., K. Hanson, S. B. Jilcott Pitts, J. Kolodinsky, M. Sitaker, A. Ammerman, R. A. Seguin. 2016. “.” Paper presented at American Public Health Association annual meeting, Denver, CO, 29 October–2 November.
Mytton, O. T., K. Nnoaham, H. Eyles, P. Scarborough, and C. N. Mhurchu. 2014. “Systematic Review and Meta-Analysis of the Effect of Increased Vegetable and Fruit Consumption on Body Weight and Energy Intake.” BMC Public Health 14,: 886.
Nesheim, M. C., M. Oria, and P. T. Yih, eds. 2015. A Framework for Assessing Effects of the Food System. Washington, DC: National Academies Press.
National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. 2012. Overweight and Obesity Statistics. Available online: http://win.niddk.nih.gov/statistics/
Northeast Organic Farming Association of Vermont. 2014. The Vermont Farm Share Program. Available online: http://nofavt.org/programs/farm-share
Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal. 2014. “Prevalence of Childhood and Adult Obesity in the United States, 2011–2012.” Journal of the American Medical Association 311: 806–814.
Perez, J., P. Allen, and M. Brown. 2003. Community Supported Agriculture on the Central Coast: The CSA Member Experience. Santa Cruz, CA: UC-Santa Cruz, The Center for Agroecology and Sustainable Food Systems, Research Brief 1, Winter.
Poti, J. M., K. J. Duffey, and B. M. Popkin. 2014. “The Association of Fast Food Consumption with Poor Dietary Outcomes and Obesity among Children: Is It the Fast Food or the Remainder of the Diet?” American Journal of Clinical Nutrition 99: 162–171.
Quandt, S. A., J. Dupuis, C. Fish, and R. B. D’Agostino, Jr. 2013. “Feasibility of Using a Community-Supported Agriculture Program to Improve Fruit and Vegetable Inventories and Consumption in an Underresourced Urban Community.” Preventing Chronic Disease 10: 1–9.
Rolls, B. J., J. A. Ello-Martin, and B. C. Tohill. 2004. “What Can Intervention Studies Tell Us about the Relationship between Fruit and Vegetable Consumption and Weight Management?” Nutrition Reviews 62: 1–17.
Russell, W. S., and L. Zepeda. 2008. “The Adaptive Consumer: Shifting Attitudes, Behavior Change and CSA Membership Renewal.” Renewable Agriculture and Food Systems 23: 136–148.
Sabih, S., and L. Baker. 2000. “Alternative Financing in Agriculture: A Case for the CSA Method.” Acta Horticulturae 524: 141–148.
Saulny, S. 2008, July 10. “Cutting Out the Middlemen, Shoppers Buy Slices of Farms.” New York Times, p. A1.
Seguin, R. A., and J. Kolodinsky. 2016. “ Paper presented at the National Association of Community Development Extension Professionals annual meeting, Burlington, VT, 26–29 June.
Seguin, R. A., A. S. Ammerman, K. L. Hanson, S. B. Jilcott Pitts, J. Kolodinsky, and M. H. Sitaker. 2016. “.” Paper presented at the Society for Nutrition Education and Behavior annual meeting, San Diego, CA, 30 July–2 August.
Sitaker, M., J. Kolodinsky, S. Jilcott Pitts, and R. Seguin 2014. “Do Entrepreneurial Food Systems Innovations Impact Rural Economies and Health? Evidence and Gaps.” Journal of Entrepreneurship 7(2): 4–15.
Stagl, S. 2002. Local Organic Food Markets: Potentials and Limitations for Contributing to Sustainable Development.” Empirica 29: 145–162.
Sturm, R. 2005. “Economics and Physical Activity: A Research Agenda.” American Journal of Preventive Medicine 28: 141–149.
Tohill, B. C., J. Seymour, M. Serdula, L. Kettel-Khan, and B. J. Rolls. 2004. “What Epidemiologic Studies Tell Us about the Relationship between Fruit and Vegetable Consumption and Body Weight.” Nutrition Reviews 62: 365–374.
U.S. Department of Agriculture. 2014. USDA Strategic Plan, FY 2014–2018. Available online: http://www.usda.gov/documents/usda-strategic-plan-fy-2014-2018.pdf
U.S. Department of Agriculture, Economic Research Service. 2014. Poverty Overview. Available online: http://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/poverty-overview.aspx#.U3P4BfldWrE
U.S. Department of Agriculture and U.S. Department of Health and Human Services. 2010. Dietary Guidelines for Americans 2010. Available online: https://health.gov/dietaryguidelines/2010/
Uribe, A. L. M., D. M. Winham, and C. M. Wharton. 2012. “Community Supported Agriculture Membership in Arizona. An Exploratory Study of Food and Sustainability Behaviours.” Appetite 59: 431–436.
Wang, W., J. Kolodinsky, and R. A. Seguin. 2016. “Identifying Reasons for Attrition from Subsidized Community Supported Agriculture Membership among Limited Resource Populations.” Paper presented at the Agriculture, Food and Human Values Society annual meeting, Scarborough, ON, Canada, 22–25 June.